Neuromuscular disorders
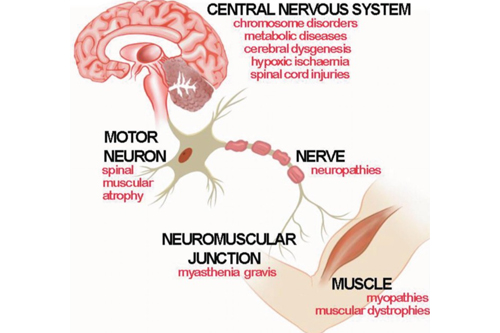
Medical conditions in Nagpur that affect the peripheral nervous system comprise various diseases of the neuromuscular system. This means all motor and sensory nerves, which link the brain and spinal cord to the rest of the body. An example is progressive muscle weakness.
Through the Neuromuscular Program, we are offering to our patients specialized evaluation and comprehensive treatment of these conditions. We are an academic tertiary care center with highly dedicated specialists, coupled with information and advances in treatment. These disorders have a very high chance of being manageable when intervention is early and appropriate.
Symptoms
Most cases of neuromuscular disorders need individualized care and are best managed by a multidisciplinary team, such as that offered at Cedars-Sinai’s Neuromuscular Disorders Program.
The commonly presenting symptoms of the condition involve slowly progressive muscle weakness and fatigue. Many conditions start at birth or in the very early years of life; however, some also begin later in childhood or even adulthood, and the onset and symptoms may vary according to the specific disorder and the site within the body affected by this disorder.
- Muscle weakness leading to twitching, cramping, and pain
- Muscle wasting
- Impaired movement
- Dysbalance disorders
- Numbness, paresthesias, or dysesthesias
- Ptosis: drooping eyelid
- Diplopia: double vision
- Dysphagia: difficulty swallowing
- Respiratory failure
How are neuromuscular disorders managed and treated?
Treatment for neuromuscular disorders is only symptomatic and aimed at slowing the progression of the disease because there is no cure yet.
Some drugs are prescribed for pain, weakness, cramps, and stiffness. Some are also administered to increase nerve impulses and muscle strength. In cases when the disorder results from autoimmune diseases, immunosuppressives can be recommended; high-dose immunoglobulin therapy can also be considered to augment antibodies.
Other treatments include:
Where there is a deficiency in the muscles, there is enhancement of muscle tone and motor skills through physical therapy. Utilization of strategies on how one can achieve daily activities while conserving energy can be developed through occupational therapy. Surgical interventions include decompression surgery to alleviate neuropathy or thymectomy to remove the thymus gland in cases of myasthenia gravis due to pressure on the nerves and other underlying conditions.
Types of Neuromuscular Disorders:
- Muscular Dystrophies (MD):
- A group of genetic disorders characterized by progressive muscle weakness or degeneration.
- Duchenne Muscular Dystrophy (DMD): The most common form, primarily affecting boys, with early onset in childhood.
- Becker Muscular Dystrophy (BMD): Similar to DMD but with a later onset or slower progression.
- Myotonic Dystrophy: Affects muscles and other body systems, including the heart and respiratory system, with prolonged muscle contractions.
- Amyotrophic Lateral Sclerosis (ALS) (Lou Gehrig’s Disease):
- A progressive neurodegenerative disorder that affects nerve cells in the brain and spinal cord, leading to muscle weakness, atrophy, and eventual paralysis.
- Typically affects voluntary muscle control, with symptoms such as difficulty speaking, swallowing, and breathing.
- Spinal Muscular Atrophy (SMA):
- A genetic disorder that affects the motor neurons in the spinal cord, leading to muscle weakness and atrophy, particularly in the legs and arms.
- SMA Type 1: The most severe form, with symptoms appearing in infancy.
- SMA Type 2 and 3: Less severe forms with later onset.
- Myasthenia Gravis (MG):
- An autoimmune disorder where antibodies block or destroy acetylcholine receptors at the neuromuscular junction, leading to muscle weakness, especially after periods of activity.
- Common symptoms include drooping eyelids (ptosis), double vision, difficulty speaking or swallowing, and generalized muscle fatigue.
- Peripheral Neuropathy:
- A condition caused by damage to peripheral nerves, leading to weakness, numbness, and pain, typically in the hands and feet.
- Can result from diabetes, infections, injuries, autoimmune diseases, or toxins.
- Guillain-Barré Syndrome (GBS):
- An autoimmune disorder in which the immune system attacks the peripheral nervous system, causing muscle weakness and sometimes paralysis.
- Often triggered by infections, GBS can progress rapidly and may require emergency medical care.
- Charcot-Marie-Tooth Disease (CMT):
- A hereditary motor and sensory neuropathy affecting peripheral nerves, leading to muscle weakness, decreased sensation, and foot deformities.
- Symptoms typically appear in adolescence or early adulthood and progress slowly.
- Polymyositis and Dermatomyositis:
- Autoimmune inflammatory diseases that cause muscle weakness, primarily in the proximal muscles (shoulders, hips, thighs).
- Dermatomyositis also involves a distinctive skin rash.
- Congenital Myopathies:
- A group of inherited muscle disorders present at birth or early childhood that cause muscle weakness and poor muscle tone.
- Includes conditions like central core disease and nemaline myopathy.
- Metabolic Myopathies:
- Muscle disorders caused by defects in the biochemical processes that produce energy in muscle cells.
- Examples include Pompe disease and McArdle’s disease.
Causes and Risk Factors:
Neuromuscular disorders can be caused by genetic mutations, autoimmune reactions, metabolic defects, or damage to the nerves due to toxins, infections, or trauma. Common causes include:
- Genetic Factors: Many neuromuscular disorders, like muscular dystrophy, SMA, and CMT, are inherited.
- Autoimmune Diseases: Disorders like myasthenia gravis and Guillain-Barré syndrome occur when the immune system attacks the body’s tissues.
- Infections: Some conditions are triggered by viral or bacterial infections (e.g., Guillain-Barré syndrome).
- Metabolic and Mitochondrial Disorders: Genetic defects in muscle energy production pathways can lead to neuromuscular problems.
Diagnosis of Neuromuscular Disorders:
Diagnosis typically involves the combination of a following:
- Physical Examination: Assessment of muscle strength, reflexes, and coordination.
- Electromyography (EMG): Measures electrical activity in muscles and can detect abnormalities in nerve or muscle function.
- Nerve Conduction Studies (NCS): Tests how well electrical signals travel along nerves.
- Muscle Biopsy: A small sample of muscle tissue is examined under a microscope to look for structural abnormalities.
- Genetic Testing: Identifies specific mutations responsible for inherited neuromuscular diseases.
- Blood Tests: Used to check for abnormal levels of muscle enzymes, autoantibodies, or other markers.
- Magnetic Resonance Imaging (MRI): Used to detect muscle or nerve damage and inflammation.
Treatment Options:
- Medications:
- Corticosteroids: Used to reduce inflammation in conditions like polymyositis or dermatomyositis.
- Immunosuppressants: For autoimmune disorders like myasthenia gravis and Guillain-Barré syndrome.
- Anticholinesterase Inhibitors: Medications like pyridostigmine can improve muscle strength in myasthenia gravis by increasing communication at the neuromuscular junction.
- Gene Therapy: Emerging therapies, such as those for SMA (e.g., Spinraza, Zolgensma), target the genetic defects that cause the disorder.
- Physical Therapy and Rehabilitation:
- Exercise: Helps maintain muscle strength, flexibility, and mobility. Exercise regimens are tailored to avoid overexertion.
- Orthotic Devices: Braces, splints, or mobility aids can help with walking and maintaining posture.
- Occupational Therapy: Helps with everyday tasks and maintaining independence.
- Breathing Assistance:
- In advanced stages of some disorders, respiratory muscles may weaken, requiring mechanical ventilation or other breathing aids.
- Surgery:
- In some cases, surgery may be required to correct deformities, such as tendon release procedures or spinal surgery for scoliosis in muscular dystrophy.
How are neuromuscular disorders diagnosed?
The assessment of reflexes and presence of muscle tone loss (atrophy) are the basic first steps to a provider when diagnosing neuromuscular disorders. Thus, some of the diagnostic tests that may help confirm the diagnosis include:
Blood tests to check various enzyme levels. Electromyography for muscle electrical activity. Imaging studies such as MRI in order to identify abnormalities in the brain and spine. Spinal tap or lumbar puncture in order to evaluate cerebrospinal fluid. First of all, Nerve conduction velocity test in which nerve-to-muscle message transduction speed is measured. In past, Muscle biopsies were taken into consideration in order to study the muscle. Genetic tests are done in order to identify inherited mutations.
At our Neurosys Multispeciality Center, we perform several key procedures including Craniotomy, which is primarily for the excision of brain tumors; V-P Shunt Surgery for treating hydrocephalus; surgeries for epilepsy; and operations targeting brain stem glioma. Beyond these, we offer a range of other neurosurgical services. If you have any questions that are not answere, please contact us through our Contact Us or Book your Appointment.
