Neurological examination
A neurological examination is a thorough physical examination aimed at identifying signs of diseases that relate to the brain, spinal cord, and nerves.
The examination often becomes the first test doctors run to analyze your nervous system’s function, thus helping decide what other tests to perform. Since every examination will be tailored to your symptoms, it might take enough time to ensure accuracy since the nervous system is quite complex.
The progress of treatment and response are evaluated by applying neurological examinations to patients suffering from pre-existing nervous system disorders.
What does a neuro exam entail?
This includes physical examinations involving functions of the nervous system, including the following:
- Ability to think and talk.
- Activity of a cranial nerves responsible for providing innervation for most parts of the head and face.
- Strength, coordination, and tone of muscles.
- Reflexes, including the knee-jerk type of reflex and others.
- Perception of different stimulation, such as touch and vibration
- Abilities or patterns of walking and general movement.
- Spinal status
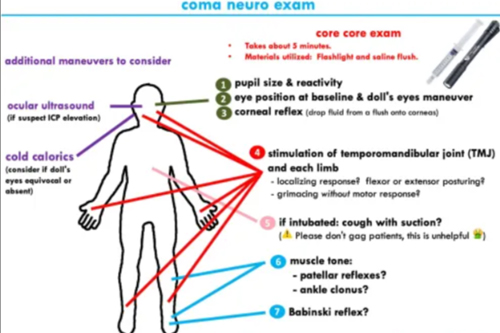
- Levels of consciousness, especially in traumatic brain injury.
Components of a Neurological Examination:
- History Taking:
- Gathering a comprehensive medical history, including symptoms, onset, duration, and any previous neurological issues.
- Reviewing personal and family medical history, medication use, and any relevant lifestyle factors.
- Mental Status Examination:
- Level of Consciousness: Assessing alertness, responsiveness, and orientation (to person, place, time).
- Cognitive Function: Evaluating memory, attention, language abilities, and executive function through tasks like recalling words, following commands, and performing simple calculations.
- Mood and Affect: Observing for signs of depression, anxiety, or other mood disorders.
- Cranial Nerve Examination:
- Assessing the function of the 12 cranial nerves, which control sensory and motor functions in the head and neck. Each nerve is tested for its specific functions:
- Olfactory Nerve (I): Sense of smell.
- Optic Nerve (II): Vision, including visual fields and acuity.
- Oculomotor Nerve (III): Eye movement and pupil reaction.
- Trochlear Nerve (IV): Eye movement (downward and inward).
- Trigeminal Nerve (V): Sensation in the face and motor function for mastication.
- Abducens Nerve (VI): Eye movement (lateral).
- Facial Nerve (VII): Facial expressions, taste (anterior two-thirds of the tongue).
- Vestibulocochlear Nerve (VIII): Hearing and balance.
- Glossopharyngeal Nerve (IX): Taste (posterior one-third of the tongue) and swallowing.
- Vagus Nerve (X): Speech, swallowing, and autonomic functions.
- Accessory Nerve (XI): Shoulder shrugging and head turning.
- Hypoglossal Nerve (XII): Tongue movement.
- Assessing the function of the 12 cranial nerves, which control sensory and motor functions in the head and neck. Each nerve is tested for its specific functions:
- Motor System Examination:
- Muscle Strength: Testing muscle strength in different muscle groups through resistance against movements.
- Muscle Tone: Assessing for hypertonia (increased tone) or hypotonia (decreased tone) during passive movement of limbs.
- Coordination and Gait: Observing the patient’s ability to perform coordinated movements (e.g., finger-to-nose, heel-to-shin) and assessing gait for balance and stability.
- Sensory System Examination:
- Light Touch: Assessing the ability to feel light touch using a cotton ball and similar object.
- Pain and Temperature: Testing pain sensation using a pin or sharp object and temperature sensation with hot and cold water.
- Vibration and Proprioception: Evaluating the sense of vibration using a tuning fork and proprioception through joint position sense (e.g., moving a toe up or down).
- Reflex Examination:
- Assessing deep tendon reflexes (e.g., knee jerk, ankle jerk) using a reflex hammer.
- Evaluating superficial reflexes (e.g., abdominal, plantar) and checking for any pathological reflexes (e.g., Babinski sign).
- Autonomic Nervous System Examination:
- Assessing blood pressure and heart rate changes while lying down or standing (orthostatic hypotension).
- Evaluating sweating patterns and pupillary responses.
Interpretation of Findings:
The results of a neurological examination can help identify neurological disorders such as:
- Stroke: Sudden onset of weakness, speech difficulties, or visual disturbances.
- Multiple Sclerosis: Signs of coordination problems, sensory changes, or vision issues.
- Parkinson’s Disease: Rigidity, bradykinesia, and tremors.
- Peripheral Neuropathy: Sensory deficits, weakness, or reflex abnormalities.
- Dementia: Memory impairment, cognitive deficits, and personality changes.
Will I need any additional tests?
If the results are not within the average range, the neurologist may require further elucidation by ordering other tests. Among the tests that may be the ordered are:
- Blood tests: ruling out other conditions like a deficiency of the either vitamin B12 or vitamin D.
- Imaging tests. Such as an MRI and CT scan.
- Electrical activity in your brain, electroencephalogram.
- Electromyogram and nerve conduction studies to evaluate nerve and muscle function.
Lumbar puncture.
At our Neurosys Multispeciality Center, we perform several key procedures including Craniotomy, which is primarily for the excision of brain tumors; V-P Shunt Surgery for treating hydrocephalus; surgeries for epilepsy; and operations targeting brain stem glioma. Beyond these, we offer a range of other neurosurgical services. If you have any questions that are not answere, please contact us through our Contact Us or Book your Appointment.
