Deep Brain Stimulation
Brain surgery involves a medical intervention meant to correct abnormalities within the brain and its surrounding structures. These structures are some of the very critical parts of the central nervous system. They are crucial in functions such as speech, movement, cognition, and memory. Conditions targeted are those that directly affect the said areas but still maintain their main functions.
There are many reasons that make brain surgery necessary. The reasons range from the need to remove part of the brain to control seizures, a tumor from the brain, surgery in order to pressure within the skull caused by excess blood or cerebrospinal fluid known as hydrocephalus and it is also applied to rectify abnormalities in the blood vessels such as aneurysms.
Although there are several benefits of brain surgery, it is not free of risk. The patients have to stay in the hospital after the treatment so that a medical team could keep close monitoring the progress of the recovery and the optimal outcome.
What conditions and symptoms can DBS treat?
DBS is now recognized as a therapeutic treatment for many disorders related to the brain – neurological movement disorders, psychiatric disorders, and epilepsy. FDA approval has been acquired for DBS therapy on the following conditions:
Dystonia.
Essential Tremor.
Drug-resistant epilepsy.
Parkinson’s disease, in cases where conventional medication proves ineffective.
Medication-resistant obsessive-compulsive disorder (OCD).
Best hospital for neurosurgery
Neurosurgery almost requires absolute precision and accuracy due to its critical nature concerning the brain and spine, where every neuron counts. Though accuracy is always required in all specialties of medicine, the risks here are considerably higher because the structures involved are delicate.
The following are key procedures we carry out at our Neurosys Multispeciality Center, including: Craniotomy V-P Shunt Surgery Handling hydrocephalus cases: Epilepsy surgeries; Also, operations that target the brain stem glioma. There are numerous other neurosurgical services that we shall offer. For those questions not yet answered, reach us through Contact Us or Book your Appointment.
Key Features of Deep Brain Stimulation:
- Reversible: Unlike lesioning procedures, DBS is reversible and adjustable, meaning the electrical stimulation can be modified, turned on or off, and the effects are non-permanent.
- Targeted Stimulation: DBS targets specific brain areas involved in movement, mood, and other neurological functions.
- Customizable: The settings of the device can be adjusted based on the patient’s symptoms and needs, allowing for tailored treatment.
Conditions Treated by Deep Brain Stimulation:
- Parkinson’s Disease
- DBS is commonly used to manage motor symptoms such as tremors, stiffness, slowness of movement (bradykinesia), and involuntary movements (dyskinesia) in patients whose symptoms are not adequately controlled with medication.
- Essential Tremor
- This is the most common movement disorder, characterized by uncontrollable shaking, typically in the hands or arms. DBS can help reduce the severity of tremors, especially in patients who do not respond to medications.
- Dystonia
- A movement disorder in which muscles contract involuntarily, causing abnormal postures or repetitive movements. DBS can reduce muscle spasms and improve motor function.
- Epilepsy
- DBS can be used as a treatment for patients with drug-resistant epilepsy to reduce the frequency and severity of seizures.
- Obsessive-Compulsive Disorder (OCD)
- For patients with severe, treatment-resistant OCD, DBS can help alleviate symptoms by targeting brain areas involved in mood regulation and compulsive behaviors.
- Tourette Syndrome
- DBS has shown promise in reducing tics and improving the quality of life for individuals with severe, treatment-resistant Tourette syndrome.
- Depression (Experimental)
- In cases of severe, treatment-resistant depression, DBS has been explored as a potential treatment, targeting areas of the brain involved in mood regulation.
How Deep Brain Stimulation Works:
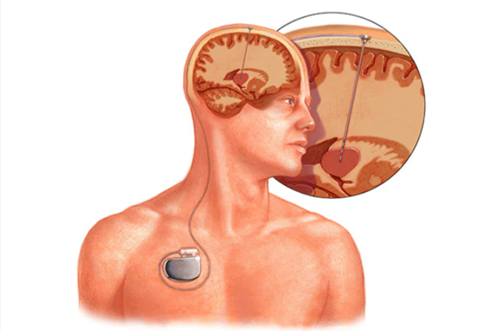
- Electrode Placement
- Electrodes are implanted into specific areas of the brain depending on the condition being treated:
- Subthalamic nucleus (STN) and globus pallidus interna (GPi) for Parkinson’s disease and dystonia.
- Thalamus for essential tremor.
- Anterior nucleus of the thalamus for epilepsy.
- Electrodes are implanted into specific areas of the brain depending on the condition being treated:
- Implantable Pulse Generator (IPG)
- The electrodes are connected to a small device called an implantable pulse generator (IPG), which is usually placed under the skin near the collarbone or in the abdomen.
- The IPG sends continuous electrical impulses to the electrodes in the brain, which help modulate abnormal activity and improve symptoms.
- Programming and Adjustment
- After surgery, the DBS system is activated, and the settings are adjusted to optimize symptom control. This process, known as “programming,” is done over several visits to ensure the electrical stimulation is tailored to the patient’s needs.
- The stimulation settings (intensity, frequency, and duration of pulses) can be fine-tuned non-invasively using a wireless controller.
- Battery Life and Recharging
- Depending on the type of IPG used, the battery may last 3 to 5 years and require surgical replacement, or it may be rechargeable and last up to 10 years before needing replacement.
What happens after Deep Brain Stimulation In Nagpur ?
After the placement of the pulse generator, your doctor will appoint follow-up in the period of a weeks, where they’ll start programming the pulse generator.
The majority of the modern pulse generators are made with an innate wireless antenna; therefore, your doctor will be able to program it outside your body. Fine tuning may take multiple visits.
Most pulse generators are fitted with specialty long-life batteries. Standard batteries have a shelf life of three to the five years, while rechargeable batteries may last from nine years. Replacing the battery again involves another surgical intervention. Such a procedure is often less traumatic and time consuming than the initial implantation. Patients often leave the hospital the same day after replacing the battery for their stimulator.
The DBS Procedure:
- Preoperative Imaging and Planning
MRI or CT scans are taken to create a detailed map of the brain and identify the exact location for electrode placement. Advanced imaging techniques help ensure accuracy and minimize risks. - Stereotactic Frame or Frameless System
A stereotactic frame may be attached to the patient’s head during surgery to guide the precise insertion of electrodes. In some cases, frameless systems are used for greater patient comfort. - Electrode Implantation (Stage 1)
The surgery is typically performed while the patient is awake (for Parkinson’s disease and essential tremor cases) so that doctors can monitor brain activity and symptoms in real time. Small holes are drilled into the skull, and electrodes are inserted into the target areas of the brain.
Neurologists may test the patient’s response during surgery by stimulating the electrodes and assessing improvements in symptoms such as tremors or rigidity. - Implantation of the Pulse Generator (Stage 2)
In a second surgical procedure, the pulse generator is implanted under the skin of the chest, and wires from the electrodes are tunneled under the skin to connect with the pulse generator. - Postoperative Programming
A few weeks after surgery, the DBS system is turned on, or the electrical stimulation settings are adjusted. This process continues over time as symptoms change or to reduce side effects like speech problems or muscle contractions.
Benefits of Deep Brain Stimulation:
- Improvement in Motor Symptoms
- DBS has been shown to significantly reduce motor symptoms in Parkinson’s disease, essential tremor, and dystonia, improving patients’ ability to perform daily activities.
- Medication Reduction
- Patients with Parkinson’s disease may be able to reduce their medication dosage, which can also reduce medication-related side effects like dyskinesia.
- Reversible and Adjustable
- Unlike some other surgical treatments (e.g., lesioning procedures), DBS is reversible and the stimulation settings can be adjusted as needed.
- Long-Term Effects
- DBS can provide sustained symptom control for several years, though periodic adjustments may be required.
Risks and Complications:
As with any surgical procedure, a DBS carries certain risks, including:
Infection: There is a small risk of infection at the site of the electrode or pulse generator.
Bleeding in the Brain: The procedure carries a risk of hemorrhage, which could lead to stroke or other neurological deficits.
Hardware Malfunctions: The electrodes or pulse generator may malfunction, requiring additional surgery for repair or replacement.
Side Effects: Electrical stimulation can cause temporary side effects such as:
– Tingling sensations
– Speech or balance problems
– Mood changes or depression
– Cognitive issues (e.g., confusion, memory difficulties)
– Psychological Effects: Some patients may experience mood changes, anxiety, or depression after DBS.
Best neurosurgeons in nagpur
What is the recovery time?
Most people need a one-day inpatient stay after surgery to have DBS leads implanted into the brain. However, discharge on the same day as surgery to place the pulse generator is often possible.
Recovery is usually three weeks. Your physician likely will have several recommendations for you during that period of time:
For two weeks post-procedure, avoid activity that includes work or household chores and sexual activity. Abstain from lifting objects heavier than 5 pounds (2.25 kilograms).
Avoid any moderate to strenuous exercises or activities for at least four to six weeks, including active exercise and physically demanding work or activities. In most patients, normal daily activity including work may be resumed during this period.
Be careful about moving and stretching, especially a few days after the surgery involving the pulse generator. You’re also supposed to avoid certain movements for some days, such as raising your arms over your head. The degree of restriction and time will depend on the doctor’s specific guidance.
