Cervical Spondylitis
For most people, cervical spondylosis causes no symptoms. When symptoms do occur, they typically include pain and stiffness in the neck.
Sometimes, cervical spondylosis results in a narrowing of the space needed by the spinal cord and the nerve roots that pass through the spine to the rest of your body. If the spinal cord or nerve roots become pinched, you might experience:
- Tingling, numbness and weakness in your arms, hands, legs or feet
- Lack of coordination and difficulty walking
- Loss of bladder or bowel control
As you age, the bones and cartilage that make up your backbone and neck gradually develop wear and tear. These changes can include:
- Dehydrated disks. Disks act like cushions between the vertebrae of your spine. By the age of 40, most people’s spinal disks begin drying out and shrinking, which allows more bone-on-bone contact between the vertebrae.
- Herniated disks. Age also affects the exterior of your spinal disks. Cracks often appear, leading to bulging (herniated) disks — which sometimes can press on the spinal cord and nerve roots.
- Bone spurs. Disk degeneration often results in the spine producing extra amounts of bone in a misguided effort to strengthen the spine. These bone spurs can sometimes pinch the spinal cord and nerve roots.
- Stiff ligaments. Ligaments are cords of tissue that connect bone to bone. Spinal ligaments can stiffen with age, making your neck less flexible.
Risk factors for cervical spondylosis include:
- Age. Cervical spondylosis is a normal part of aging.
- Occupation. Jobs that involve repetitive neck motions, awkward positioning or a lot of overhead work put extra stress on your neck.
- Neck injuries. Previous neck injuries appear to increase the risk of cervical spondylosis.
- Genetic factors. Some individuals in certain families will experience more of these changes over time, while others will not.
- Smoking. Smoking has been linked to increased neck pain
If your spinal cord or nerve roots become severely compressed as a result of cervical spondylosis, the damage can be permanent.
Your doctor will likely start with a physical exam that includes:
- Checking the range of motion in your neck
- Testing your reflexes and muscle strength to find out if there’s pressure on your spinal nerves or spinal cord
- Watching you walk to see if spinal compression is affecting your gait
Imaging tests
Imaging tests can provide detailed information to guide diagnosis and treatment. Your doctor might recommend:
- Neck X-ray. An X-ray can show abnormalities, such as bone spurs, that indicate cervical spondylosis. Neck X-ray can also rule out rare and more serious causes for neck pain and stiffness, such as tumors, infections or fractures.
- CT scan. A CT scan can provide more detailed imaging, particularly of bones.
- MRI. MRI can help pinpoint areas where nerves might be pinched.
- Myelography. A tracer dye is injected into the spinal canal to provide more detailed X-ray or CT imaging.
Nerve function tests
Your doctor might recommend tests to determine if nerve signals are traveling properly to your muscles. Nerve function tests include:
- Electromyography. This test measures the electrical activity in your nerves as they transmit messages to your muscles when the muscles are contracting and at rest.
- Nerve conduction study. Electrodes are attached to your skin above the nerve to be studied. A small shock is passed through the nerve to measure the strength and speed of nerve signals.
Treatment for cervical spondylosis depends on the severity of your signs and symptoms. The goal of treatment is to relieve pain, help you maintain your usual activities as much as possible, and prevent permanent injury to the spinal cord and nerves.
Medications
If over-the-counter pain relievers aren’t enough, your doctor might prescribe:
- Nonsteroidal anti-inflammatory drugs. While some types of NSAIDs are available over the counter, you may need prescription-strength versions to relieve the pain and inflammation associated with cervical spondylosis.
- Corticosteroids. A short course of oral prednisone might help ease pain. If your pain is severe, steroid injections may be helpful.
- Muscle relaxants. Certain drugs, such as cyclobenzaprine, can help relieve muscle spasms in the neck.
- Anti-seizure medications. Some epilepsy medications, such as gabapentin (Neurontin, Horizant) and pregabalin (Lyrica), can dull the pain of damaged nerves.
- Antidepressants. Certain antidepressant medications have been found to help ease neck pain from cervical spondylosis.
Therapy
A physical therapist can teach you exercises to help stretch and strengthen the muscles in your neck and shoulders. Some people with cervical spondylosis benefit from the use of traction, which can help provide more space within the spine if nerve roots are being pinched.
Surgery
If conservative treatment fails or if your neurological signs and symptoms — such as weakness in your arms or legs — worsen, you might need surgery to create more room for your spinal cord and nerve roots.
The surgery might involve:
- Removing a herniated disk or bone spurs
- Removing part of a vertebra
- Fusing a segment of the neck using bone graft and hardware
Lumbar Spondylitis
Lumbar spondylosis is the term given to normal wear and tear of the lumbar (lower back) spinal discs. As we age, spinal discs lose moisture and shrink, bone spurs develop, and bones because weaker. While many people over 50 experience mild lumbar spondylosis, most experience no symptoms.
If you are experiencing symptoms, it likely means the condition is progressing and could cause other, more serious spinal conditions.
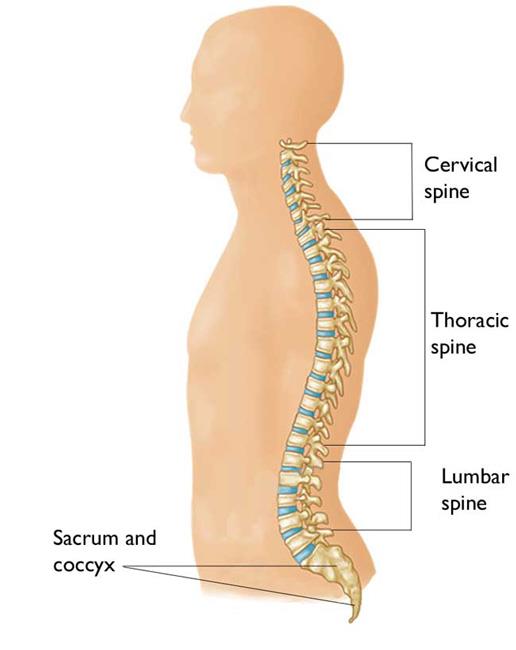
Since the purpose of the lumbar spine is to support your body weight, over time the L1-S1 vertebrae become worn and compressed from repetitive motion, heavy lifting, and weight gain.
Common causes include:
- Herniated or bulging discs
- Bone spurs
- Spine abnormalities
- Arthritis of the spine
In most cases, lumbar spondylosis only causes noticeable symptoms when the spinal cord or nerves around the spine become irritated or compressed. When symptoms do occur, they can differ greatly from person to person. For example, if there is pressure on the sciatic nerve, it can cause pain in the back, buttocks, legs, feet, and toes.
Common symptoms of lumbar spondylosis that may vary from case to case include:
- Intermittent back pain that may radiate to the extremities
- Joint or muscular stiffness upon awakening
- Muscle weakness and/or tingling in the back, buttocks, legs, and other affected areas
- Numbness or loss of sensation in the affected areas
- Tenderness in the area of nerve compression
- Loss of bowel or bladder control
In addition to a physical exam to note range of motion, reflexes, and fine motor skills, the spine specialists at Kelsey-Seybold Spine Center can perform imaging and other tests to determine the exact cause of your symptoms and what treatment is appropriate.
These tests may include:
- X-rays of the back to discover any abnormalities
- CT scan for more detailed imaging of bones
- MRI to find any areas where nerves may be compressed
- Myelography in which a dye is injected into the spinal canal prior to imaging tests
- A nerve function test called electromyography (EMG) that tests electrical activity in your nerves
- A nerve conduction study during which electrodes attached to the skin measures strength and speed of nerve signals
Treatment for lumbar spondylosis depends on the severity of your symptoms. Our spine specialists will develop a treatment plan to relieve your pain, avoid future damage, and help you manage your condition.
This treatment plan may include nonsurgical options, including:
- Physical therapy
- Restorative yoga
- Lifestyle changes, such as weight loss
- Pain medication and trigger point injections
In cases when nonsurgical treatment doesn’t relieve symptoms, we may suggest minimally invasive surgery to decompress the spine.
Almost everyone develops lumbar spondylosis at some point, but not everyone experiences symptoms. If you have chronic back stiffness and pain that may radiate down your buttocks and legs, the team at Kelsey-Seybold Spine Center in Houston can determine if lumbar spondylosis is the cause and what treatment.