Cervical cancer screening
This cervical cancer screening in Nagpur is vital health practice meant to detect cervical cancer in the female population. The following are the key points covered in the main discussion
Screening tests
1. Pap test (Pap smear): collects cells from cervix to be examined for abnormality.
2. HPV test: High-risk types of HPV that may be associated with cervical cancers can be identified.
3. Co-testing: a combination of a Pap test with an HPV test for improved and accurate results.
Screening Recommendations:
1. Start Screening at Age 21.
2. Screen Every 3 Years with Pap test alone and every 5 years with co-testing.
3. Stop Screening at Age 65 if normal results and no history of cervical cancer.
Who Should be Screened:
1. Women Aged 21-65 Years.
2. Women having a Cervix, irrespective of her sexual activity.
3. Women with history of cervical cancer, HPV and abnormal Pap tests.
Why Should One be Screened?
1. Cervical Cancer may be avoided with early detection and treatment.
2. Saves cervical cancer deaths
3. It aids in the detection of precursor cells that may be treated at an early stage.
More Tips:
1. You must get screened regularly even after you have been vaccinated against the virus causing HPV.
2. Share your history of screening as well as any issues with your doctor.
3. Do not ever run away or fear to get screened for cervical cancer because that thing is quite fast and painless!
Remember, cervical cancer screening is an important part of women’s healthy living. Keep track and go to your healthcare provider for advice on what best fits you!
What Is a Cervical cancer screening?
Such a cervical screening test is a medical check-up to detect abnormal cells in the cervix, which could eventually become cancerous. The screening identifies precancerous cells or early-stage cancer that can cervical cancer can be the treated for prior to developing.
There are two types of a cervical cancer screening tests are:
1. Pap Test (Pap Smear): A procedure to obtain cells from the cervix that, upon microscopic examination, will check for changes that are indicative of abnormal cell changes.
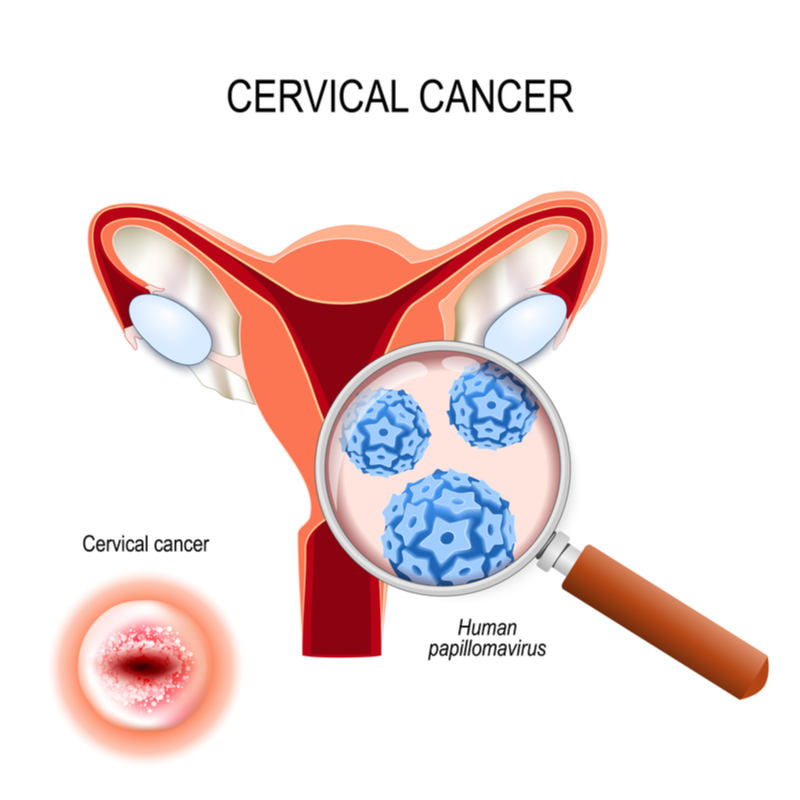
2. Human Papillomavirus (HPV) Test: A test to detect high-risk HPV types in the cervix, as this may result in cervical cancer.
The screening often involves the following procedures;
1. A pelvic exam
2. Insertion of a speculum for cervical visualization
3. Collecting cells from the cervix using spatula and/or brush
4. Cell transmission to the laboratory for testing
Women between the ages of 21-65 years should undergo regular cervical cancer screening. General recommendations include in a screening every three years using only a Pap test and co-testing (the use of both Pap or HPV tests) every five years.
Early detection and treatment improve outcomes and survival.
Importance of Cervical Cancer Screening
Cervical cancer screening helps identify:
- Precancerous changes: Abnormal cervical cells (called cervical dysplasia) that could develop into cancer if left untreated.
- Early-stage cervical cancer: Detecting cancer in its early stages increases the chances of successful treatment.
- HPV infection: Persistent infection with high-risk HPV types is the leading cause of cervical cancer.
Screening Methods
- Pap Smear (Pap Test):
- Purpose: To detect abnormal changes in the cervical cells.
- Procedure: A healthcare provider uses a small brush or spatula to gently scrape cells from the cervix. These cells are then examined under the microscope to a check for the abnormalities.
- Frequency:
- Women aged 21 to 29 should have the Pap smear every 3 years.
- Women aged 30 to 65 should have a Pap smear every 3 years, or they can opt for combined Pap and HPV testing every 5 years.
- Results:
- Normal: No abnormal cells are found.
- Abnormal: The presence of abnormal cells may require further testing, such as a repeat Pap smear, colposcopy, or biopsy.
- HPV Testing:
- Purpose: To detect high-risk strains of HPV, particularly those that are most commonly linked to cervical cancer (e.g., HPV-16, HPV-18).
- Procedure: Similar to a Pap smear, cells from the cervix are collected and tested specifically for the presence of high-risk HPV strains.
- Frequency:
- Women aged 30 to 65 can be screened with an HPV test alone every 5 years or in combination with a Pap smear.
- Results:
- Negative: No high-risk HPV strains are detected.
- Positive: High-risk HPV is present, but this doesn’t necessarily mean cancer is present. Further monitoring or testing may be recommended.
- Co-testing (Pap + HPV Test):
- Combining both the Pap smear and HPV testing provides a more comprehensive screening approach, offering better detection rates for women aged 30 and above.
Who Should Get Screened?
- Women aged 21-29: Pap smear every 3 years; HPV testing is not recommended unless the Pap smear is abnormal.
- Women aged 30-65: Pap smear every 3 years, HPV test every 5 years, or both (co-testing) every 5 years.
- Women over 65: If they have had regular normal screening results for a past 10 years or a no history of cervical pre-cancer, they may stop screening.
- Women who have had a hysterectomy: Screening may not be necessary if the cervix has been removed and there is no history of cervical cancer or precancerous conditions.
Special Considerations
- HPV Vaccination: Women who have received the HPV vaccine should still undergo routine cervical cancer screening, as the vaccine does not protect against all cancer-causing HPV strains.
- HIV or Immunocompromised Individuals: Women with weakened immune systems may need more frequent screening.
- History of Abnormal Results: Women with previous abnormal Pap smears may require closer monitoring and more frequent screening.
Abnormal Pap Smear Results
An abnormal Pap smear doesn’t necessarily mean cancer. Some possible abnormal results include:
- Atypical Squamous Cells (ASC): Minor cell changes that may or may not be related to HPV.
- Low-Grade Squamous Intraepithelial Lesion (LSIL): Mild abnormalities, often caused by HPV.
- High-Grade Squamous Intraepithelial Lesion (HSIL): More serious changes that could lead to cervical cancer if not treated.
- Atypical Glandular Cells (AGC): Abnormal glandular cells that may indicate more serious conditions, including cancer.
Prevention and Risk Reduction
- HPV Vaccine Infection: Vaccines like Gardasil and Cervarix protect against all the high-risk HPV strains which cause most cases of cervical cancers.
- Safe Sexual Practices: Safe sexual practices like condom use and the reduction of sexual partners greatly reduce the risk of infection with the HPV virus.
- Regular Screening: The best prevention of cervical cancer is early detection by regular Pap smears as well as testing for the human papilloma virus.
What procedures Cervical cancer screening?
The procedures for cervical cancer screening are as follows:
1. Pap Test or Pap Smear
A speculum is inserted up to the visualization of the cervix into the vagina. The cervical cells are collected using either a spatula or a brush. Specimens are then sent to the laboratory for a examination.
2. HPV (Human Papillomavirus) Test
A sample of cervical cells is obtained through the use of a spatula or a brush.
Sample is sent to the laboratory for testing of the high-risk types of HPV
3. Co-Testing
Pap or HPV tests are combined
4. Liquid-Based Cytology
Liquid solution used in the collection and preservation of cervical cells.
5. Visual Inspection with Acetic Acid
Acetic acid applied on the cervix, abnormal cells appear.
6. Cervicography
Photograph of the cervix by taking a picture in case abnormalities are found.
7. Colposcopy:
Magnifying Instrument Examination of the cervix for abnormal cells – A magnifying instrument is used to look at the cervix for abnormal cells. 8. Biopsy: Part of cervical tissue removed for examination. These tests are very useful for diagnosis of cervical carcinoma and precancerous lesions. Follow the advice of a professional and consult a health care provider for individualized recommendations.
At our Neurosys Multispeciality Center, we perform several key procedures including Craniotomy, which is primarily for the excision of brain tumors; V-P Shunt Surgery for treating hydrocephalus; surgeries for epilepsy; and operations targeting brain stem glioma. Beyond these, we offer a range of other neurosurgical services. If you have any questions that are not answere, please contact us through our Contact Us or Book your Appointment.
