Placental disorders
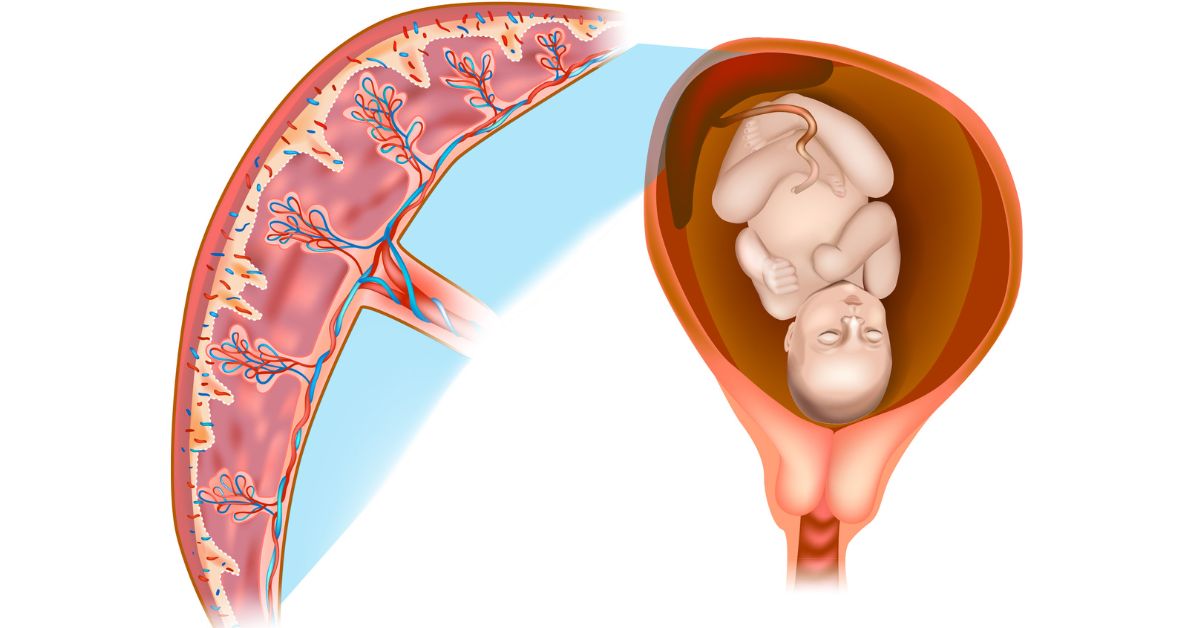
Disorders with Placental Problems in Nagpur Disorders that affect the placenta, that is an important, vermicellate and sausage-shaped organ which grows in the uterus during pregnancy, providing the fetus with the entire set of:
1. Oxygen and nutrients
2. Purification of the fetus
3. Hormone Production for Maintenance of Pregnancy
Hormonal diseases may result due to abnormalities in the placenta that could compromise the development and growth of the fetus and thereby trouble it at birthtime, while it is being delivered, and even after the delivery.
Disorders of the placenta are conditions that will lead to complications during pregnancy, delivery, and post delivery. Some common disorders of the placenta include:
1. Placenta Previa
2. Placental Abruption
3. Placenta Accreta
4. Placental Insufficiency
5. Chorioamnionitis
6. Placental Infarction
7. Placental Calcification
8. Placental Hemorrhage
9. Placental Insufficiency with Fetal Growth Restriction
10. Placental Dysfunction
All these disorders have sub complications including:
Bleeding and hemorrhage
Fetal growth restriction
Fetal distress
Preterm birth
Low birth weight
Stillbirth
Proper prenatal care should be followed by a pregnant woman so the condition of the placenta may be closely observed for any disorders that may develop.
What Is a Placental disorders?
Placental disorders are complications in a very sensitive organ of the human body that develops in the uterus when a lady is pregnant. The placenta performs a very vital role as it is crucial to the following practices:
1. provides oxygen and nutrients to the fetus
2. It removes waste products from a fetus
3. Hormones necessary for pregnancy are produced
Placental disorders would most likely disrupt these activities, thereby allowing complications to arise between the mother and the fetus. These disorders can be associated with:
1. Placental development or structure
2. Placental function or perfusion
3. Placental attachment or separation
4. Infections or inflammation
5. Maternal or fetal vascular issues
Among the most common placental disorders, there is placenta previa, placental abruption, placenta accreta, and placental insufficiency. All these conditions are closely monitored and managed by the health care providers for a positive outcome of pregnancy.
Here are the key placental disorders:
1. Placenta Previa
- Description: Occurs when the placenta implants in the lower part of the uterus and covers part and all of the cervix.
- Types:
- Complete Placenta Previa: Fully covers the cervix.
- Partial/Marginal Previa: Partially covers and is close to the cervix.
- Symptoms: Painless vaginal bleeding in the second or third trimester.
- Complications: Preterm birth, heavy bleeding (hemorrhage) during pregnancy or delivery, and the need for cesarean section.
- Management: Bed rest, monitoring, and planned cesarean delivery in severe cases.
2. Placental Abruption (Abruptio Placentae)
- Description: The placenta partially or completely separates from the uterine wall before delivery.
- Symptoms: Sudden vaginal bleeding, abdominal pain, or uterine tenderness.
- Risks: Fetal distress, preterm birth, stillbirth, or severe maternal bleeding.
- Risk Factors: Trauma, high blood pressure, preeclampsia, smoking, substance abuse, and previous placental abruption.
- Management: Immediate medical intervention; in severe cases, emergency delivery may be required.
3. Placenta Accreta Spectrum
- Description: The placenta grows too deeply into the uterine wall, making it difficult to detach after delivery.
- Types:
- Placenta Accreta: Attaches too deeply but does not invade muscle.
- Placenta Increta: Invades the uterine muscle.
- Placenta Percreta: Penetrates the uterine wall and sometimes into other organs like the bladder.
- Symptoms: Heavy bleeding during delivery or after birth.
- Risks: Severe hemorrhage, often requiring a hysterectomy to control bleeding.
- Risk Factors: Previous cesarean sections, placenta previa, uterine surgeries.
- Management: Planned cesarean delivery and potential hysterectomy.
4. Vasa Previa
- Description: Fetal blood vessels run across or near the cervix, unprotected by the umbilical cord or placenta.
- Symptoms: Often detected during routine ultrasound; vaginal bleeding and fetal distress during labor.
- Risks: Rupture of the vessels can cause severe fetal blood loss, leading to life-threatening complications for the baby.
- Management: Early diagnosis through ultrasound and scheduled cesarean delivery before labor to prevent vessel rupture.
5. Placental Insufficiency (Uteroplacental Insufficiency)
- Description: The placenta cannot deliver enough oxygen or nutrients to the fetus, affecting growth and development.
- Symptoms: Fetal growth restriction (IUGR), reduced amniotic fluid, and decreased fetal movements.
- Risks: Low birth weight, preterm birth, fetal distress, and stillbirth.
- Risk Factors: Preeclampsia, maternal hypertension, diabetes, smoking, and advanced maternal age.
- Management: Regular monitoring of fetal growth and amniotic fluid; early delivery may be required in severe cases.
6. Chorioamnionitis
- Description: Infection of the placenta and amniotic fluid.
- Symptoms: Fever, uterine tenderness, foul-smelling vaginal discharge, and rapid heart rate (maternal and fetal).
- Risks: Preterm birth, fetal infection, sepsis, and neonatal complications.
- Risk Factors: Premature rupture of membranes (PROM), prolonged labor, multiple vaginal exams.
- Management: Antibiotic treatment and delivery, depending on the severity and stage of pregnancy.
7. Molar Pregnancy (Hydatidiform Mole)
- Description: Abnormal tissue growth in the uterus, often without a viable fetus, as part of gestational trophoblastic disease.
- Types:
- Complete Mole: No fetal tissue, only abnormal placental growth.
- Partial Mole: Abnormal growth along with some fetal tissue.
- Symptoms: Vaginal bleeding, rapid uterine growth, severe nausea, and high hCG levels.
- Risks: Can develop into persistent gestational trophoblastic disease or choriocarcinoma (cancer).
- Management: Evacuation of the uterus and monitoring of hCG levels for recurrence.
8. Placental Calcification
- Description: Calcium deposits form in the placenta, usually seen in the later stages of the pregnancy as the placenta ages.
- Symptoms: Often asymptomatic, detected via ultrasound.
- Risks: Premature calcification may lead to the placental insufficiency or fetal growth restriction.
- Management: Monitoring of fetal growth and placental function; early delivery if placental aging affects fetal health.
Risk Factors for Placental Disorders:
- Maternal Age: Advanced maternal age (over 35) increases the risk of placental disorders.
- Previous Placental Complications: History of placental disorders raises the likelihood of recurrence.
- Multiple Pregnancies: Women carrying twins or higher multiples are at greater risk.
- Lifestyle Factors: Smoking, drug use, and poor prenatal care contribute to higher risks.
- Medical Conditions: High blood pressure, diabetes, and previous uterine surgeries like cesarean sections are associated with increased risk.
What procedures Placental disorders?
Disorders in the placenta require different approaches to their diagnosis, follow-up, and management. Some of the most common approaches include the following:
1. Ultrasound: The method that allows visualization of the placenta, examination for any abnormality, and assessment of fetal growth.
2. Doppler Studies: Evaluation of blood flow in the umbilical cord and the placenta.
3. Non-Stress Test (NST): An estimate of fetal well-being and measure of distress.
4. Biophysical Profile (BPP): Evaluation of fetal well-being and placental function.
5. Amniocentesis: It takes amniotic fluid sample for infection or other abnormalities testings.
6. CVS: Chorionic villus sampling is done for the examination of genetic disorders and tissue sampling from the placenta.
7. Placental Cortical Sampling: This is used to detect abnormalities in the tissues of the placenta.
8. Fetal Heart Rate Monitoring: This is checked and monitored to observe the fetal heart rate and detect any anomalies.
9. Maternal Blood Tests: These are tests to detect infection, inflammation, or other problems within the placenta itself.
10. Tests of Placental Dysfunction: These tests check on the functionality of the placenta as well as any deficiency of it.
11. Fetal growth ultrasound: to evaluate for restriction
12. Emergency delivery due to placental abruption: this is an emergent delivery in case of a placental abruption emergency.
These are diagnostic and treatment measures for the disorder, hence best results achievable for both mother and baby.
At our Neurosys Multispeciality Center, we perform several key procedures including Craniotomy, which is primarily for the excision of brain tumors; V-P Shunt Surgery for treating hydrocephalus; surgeries for epilepsy; and operations targeting brain stem glioma. Beyond these, we offer a range of other neurosurgical services. If you have any questions that are not answere, please contact us through our Contact Us or Book your Appointment.
