Fetal growth restriction
Fetal growth restriction in nagpur is a condition where the fetus does not gain the usual weight inside the womb. It is also called as a intrauterine growth restriction (IUGR).
Causes:
1. Placental insufficiency
2. Maternal hypertension
3. Preeclampsia
4. Diabetes
5. Kidney disease
Symptoms:
1. Having a lesser size for a gestational age
2. Having low birth weight
3. Reducing growth of the fetus
4. Reducing movements of the fetus
5. Abnormal heart rate of the fetus
Diagnosis:
1. Measurement by ultrasound
2. Estimation of fetal weight
3. Doppler study
4. Fetal monitoring
Management:
1. Monitoring
2. Fetal surveillance
3. Bed rest or hospitalization
4. Administration of corticosteroids for lung maturity
5. Planned delivery
6. Cesarean delivery (C-section)
Complications
1. Low birth weight
2. Premature delivery
3. Fetal distress
4. Stillbirth
5. Neonatal complications
It is therefore essential to closely follow up with a health provider in the management of FGR for the best potential outcome of the fetus.
What Is a Fetal growth restriction?
Fetal growth restriction, otherwise known as a intrauterine growth restriction (IUGR), is a condition where the fetus does not grow at a normal rate inside the womb, resulting in having a smaller size that is less than the expected dimension for the gestational age.
There are many causes of FGR. These include but not limited to:
1. Placental insufficiency
2. Maternal hypertension
3. Preeclampsia
4. Diabetes
5. Kidney disease
6. Chromosomal abnormalities
7. Infections
8. Substance abuse
9. Smoking
Complications can develop from FGR. Some of these complications include:
1. Birth weight < 2,500 g
2. Delivery ≥ 37 weeks of gestation
3. Non-reassuring fetal status
4. Stillbirth after any delivery of conception products
5. Neonatal distress
FGR is diagnosed by a ultrasound measurements followed by the fetal surveillance. Management is made by monitoring closely, instillation of corticosteroids for maturation of lungs, and planned delivery which can be C-section.
It is crucial collaboration in managing FGR since it would go a long way into ensuring good results for the fetus. Early detection of FGR and its proper treatment would greatly reduce the risk factors accompanying such a condition.
Types of Fetal Growth Restriction
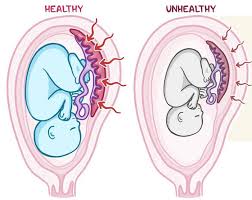
- Symmetric FGR:
- The fetus is proportionately smaller in all dimensions (head, abdomen, and limbs).
- This type usually indicates early issues during pregnancy, such as chromosomal abnormalities or congenital infections.
- Asymmetric FGR:
- The fetus has a normal-sized head but a smaller abdomen or a limbs.
- This often occurs later in pregnancy and is usually related to placental insufficiency or other maternal factors.
Causes of Fetal Growth Restriction
-
- Placental Insufficiency:
- Reduced blood flow or nutrient delivery to the fetus due to problems with the placenta, such as placental abruption, placenta previa, or abnormalities in placental structure.
- Maternal Factors:
- Chronic Conditions: Maternal health issues, such as hypertension, diabetes, heart disease, or kidney disease.
- Lifestyle Factors: Smoking, alcohol consumption, and drug use during pregnancy can negatively affect fetal growth.
- Nutritional Deficiencies: Inadequate maternal nutrition can limit the resources available for fetal growth.
- Infections:
- Maternal infections, such as cytomegalovirus (CMV), rubella, or syphilis, can lead to fetal growth restrictions.
- Genetic Factors:
- Chromosomal abnormalities or genetic syndromes in the fetus can impede normal growth.
- Multiple Pregnancies:
- Twins or higher-order multiples may experience growth restrictions due to limited space and resources.
- Placental Insufficiency:
Diagnosis of Fetal Growth Restriction
FGR is typically diagnosed through:
- Ultrasound:
- Measurement of fetal growth parameters, including abdominal circumference, head circumference, and femur length.
- Evaluation of amniotic fluid levels and placental health.
- Doppler Studies:
- Doppler ultrasound can assess blood flow in the umbilical artery and other vessels, providing information about placental function and fetal well-being.
- Non-Stress Test (NST):
- Monitoring fetal heart rate in response to fetal movements to assess fetal well-being.
- Biophysical Profile (BPP):
- Combines ultrasound and fetal heart rate monitoring to evaluate fetal health through a scoring system based on a movement, tone, breathing, or amniotic fluid volume.
Management of Fetal Growth Restriction
- Monitoring:
- Frequent ultrasounds and non-stress tests to monitor fetal growth and well-being.
- Maternal Care:
- Addressing underlying maternal health issues and promoting healthy lifestyle choices.
- Nutritional counseling to ensure adequate maternal nutrition.
- Timing of Delivery:
- If FGR is severe or there are signs of fetal distress, early delivery may be recommended, often by cesarean section if necessary.
- Postnatal Care:
- Close monitoring of the newborn after birth for potential complications related to growth restriction, including hypoglycemia, hypothermia, and feeding difficulties.
- Neonatal care may include additional interventions if the baby requires support.
What procedures Fetal growth restriction?
Fetal growth restriction should be monitored closely to manage the situation as best as possible for the fetus. The following can be done:
1. Ultrasound scans
-At least weekly or bi-weekly scanning to determine fetal growth and well-being.
-Doppler studies to evaluate blood flow and placental function.
2. Fetal surveillance
-NST to monitor the fetal heart rate.
-CST to monitor fetal heart rate for contractions.
3. Fetal Monitoring
Cardiotocography (CTG): Record of fetal heart rate and contractions
4. Amniocentesis: Determining infections and chromosomal abnormalities
5. Chorionic villus sampling (CVS): To determine whether some chromosomal abnormalities
6. Placental function tests: Determining the placental function and blood flow
7. Fetal growth scans: To predict fetal weight and to check its growth
8. Corticosteroids, to induce maturity for the baby’s lungs
9. Planned delivery: Expected way of delivery, either C-section or operative vaginal delivery
10. Puerperal care:
Intensive surveillance for complications in the infant.
These cares are scheduled for:
1. Monitoring fetal development and condition.
2. Detection of any potential complication.
3. Monitoring FGR to prevent further restriction.
4. Ensuring a healthy outcome for the fetus.
5. Planning for a proper delivery along with postpartum care for the mother.
Important information: The process and how often the cares will be done differ from one case to another depending on the physician’s instructions.
At our Neurosys Multispeciality Center, we perform several key procedures including Craniotomy, which is primarily for the excision of brain tumors; V-P Shunt Surgery for treating hydrocephalus; surgeries for epilepsy; and operations targeting brain stem glioma. Beyond these, we offer a range of other neurosurgical services. If you have any questions that are not answere, please contact us through our Contact Us or Book your Appointment.
