Neurosurgical innovations
Neurosurgical innovations In Nagpur! That the advent of Augmented Reality (AR) and Virtual Reality (VR) has turned the neurosurgical world upside down with incredible promise ! These tools enhance neurosurgery training in the trainees and aid in pain control after neurosurgical interventions .
Their promises involve global neurosurgery, especially in the Low- and Middle-Income Countries (LMICs), despite the pandemic. AR and VR have become critical instruments for hastening the neurosurgical capability across the world.
What are VR and AR?
Future Possibilities and Combinations
AR and VR can be used to supplement tools that are already in neurosurgery to overcome the limitations of what they currently provide. For instance, supplementing AR with ultrasound overcomes this limitation because AR improves the planning in the preparation stage of surgery. A pilot study revealed that if AR is supplemented with ultrasound, then pathology and anatomy are visualized more accurately than when AR is used in isolation. The use of AR supplemented with robotics has improved processes that take place in surgery as they provide critical data from auditory, visual, and tactile cues. VR is a training tool for neurosurgical trainees to become skilled in using robotics for complicated procedures as these more and more become common in the operating room.
1. Minimally Invasive Neurosurgery (MIS)
- Minimally invasive neurosurgery techniques involve smaller incisions, less tissue disruption, and quicker recovery times compared to traditional open surgery. These techniques are used for conditions like brain tumors, aneurysms, and spinal disorders.
- Endoscopic Neurosurgery: Utilizes small cameras (endoscopes) inserted through tiny incisions to navigate and operate in the brain or spine with less damage to surrounding tissue. For example, endoscopic third ventriculostomy (ETV) is commonly used to treat hydrocephalus.
- Keyhole Surgery: A type of MIS where only a small incision is made, typically in procedures such as keyhole craniotomies for brain tumor resections.
2. Neuronavigation Systems
- Neuronavigation technology is akin to GPS for the brain. It helps surgeons navigate the intricate anatomy of the brain and spine with extreme precision during surgery.
- Image-Guided Surgery (IGS): Combines preoperative imaging (like MRI or CT scans) with real-time data to provide 3D visual maps that guide surgeons. This reduces the risk of damaging healthy tissue and improves accuracy in tumor removal and other delicate procedures.
- Intraoperative MRI (iMRI): Allows surgeons to take real-time MRI images during surgery to ensure complete removal of brain tumors or to confirm the success of other procedures.
3. Robotic-Assisted Neurosurgery
- Robotics is revolutionizing neurosurgery by enhancing precision, stability, and dexterity during complex procedures.
- Robotic Stereotactic Surgery: Robots help perform precise brain surgeries like deep brain stimulation (DBS) or biopsy of deep-seated brain lesions by allowing surgeons to target specific areas with minimal error.
- Spinal Robotics: Used in spinal fusion, deformity correction, and disc replacement, spinal robotic systems assist in placing screws and hardware more accurately than conventional methods.
4. Stereotactic Radiosurgery (SRS)
- Stereotactic radiosurgery delivers highly focused radiation beams to treat brain tumors, vascular malformations, and functional disorders without the need for open surgery.
- Gamma Knife: A non-invasive radiosurgical tool that uses gamma radiation to precisely target brain lesions, often used to treat conditions like arteriovenous malformations (AVMs), acoustic neuromas, and trigeminal neuralgia.
- CyberKnife: A robotic radiosurgery system that delivers precise, high-dose radiation to tumors or other lesions anywhere in the body, including the brain and spine.
5. Awake Brain Surgery (Intraoperative Mapping)
- Awake craniotomy allows surgeons to operate on brain areas related to language, movement, and cognition while the patient is awake and responsive. This approach is critical for removing tumors near or within eloquent areas of the brain without affecting crucial functions.
- Intraoperative brain mapping during surgery helps surgeons identify and preserve important functional areas of the brain.
6. Laser Interstitial Thermal Therapy (LITT)
- LITT uses focused laser energy to heat and destroy abnormal tissue, such as tumors or epilepsy-causing lesions, with minimal impact on surrounding healthy tissue. Guided by MRI, LITT is a minimally invasive option for treating small, deep-seated brain tumors, radiation necrosis, and epilepsy.
7. Neurostimulation Devices
- Deep Brain Stimulation (DBS): DBS involves implanting electrodes in specific areas of the brain to modulate abnormal electrical activity. It is commonly used to treat movement disorders like Parkinson’s disease, dystonia, and essential tremor, and has expanded to psychiatric disorders such as depression and OCD.
- Vagus Nerve Stimulation (VNS): VNS uses electrical stimulation of the vagus nerve to treat epilepsy and depression in cases where medication fails.
- Responsive Neurostimulation (RNS): RNS is an implanted device that monitors brain activity and delivers targeted electrical stimulation to prevent seizures in patients with epilepsy.
8. 3D Printing in Neurosurgery
- 3D printing allows for the creation of patient-specific anatomical models, which are used for surgical planning, rehearsal, and custom implant design.
- Surgeons can use 3D-printed models to simulate complex surgeries on the brain or spine, ensuring greater accuracy and safety. Custom 3D-printed implants are also used for skull reconstruction after traumatic injuries or tumor resections.
9. Intraoperative Optical Imaging
- Optical imaging technologies, such as intraoperative fluorescence imaging, help surgeons distinguish between healthy and diseased tissue.
- Fluorescence-Guided Surgery: Involves injecting the patient with a fluorescent dye that accumulates in tumor cells, making them glow under specific light during surgery. This helps neurosurgeons ensure complete tumor resection.
- Intraoperative OCT (Optical Coherence Tomography): Used during spinal surgery to visualize nerve roots and ensure precise decompression.
10. Artificial Intelligence (AI) and Machine Learning
- AI is increasingly used in neurosurgery for diagnosing conditions, surgical planning, and outcome prediction.
- AI-Based Diagnosis: AI algorithms can analyze large amounts of data from imaging studies to assist in diagnosing brain tumors, vascular malformations, and other neurosurgical conditions.
- Surgical Planning and Outcome Prediction: AI models are used to predict surgical outcomes, identify optimal surgical approaches, and even anticipate complications, helping to improve patient care.
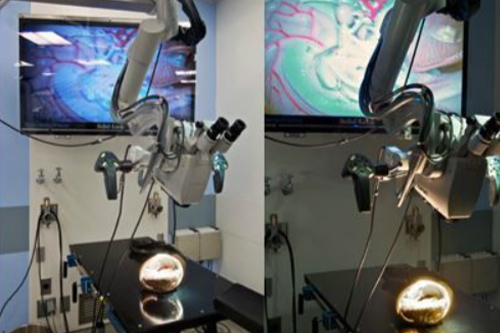
11. Augmented Reality (AR) and Virtual Reality (VR)
- AR and VR are being integrated into neurosurgery for preoperative planning, intraoperative navigation, and training.
- Augmented Reality: Projects 3D images of a patient’s brain or spine anatomy onto the surgeon’s field of view during surgery, providing real-time, enhanced visualization of critical structures.
- Virtual Reality: VR platforms are used for neurosurgical training, allowing surgeons to practice complex procedures in a virtual environment before performing them in the operating room.
12. Biomaterials and Neuroregenerative Technologies
- Advances in biomaterials are enhancing nerve repair and regeneration, particularly in spinal cord injury and peripheral nerve damage.
- Neuroregenerative Biomaterials: Materials such as nerve guides, scaffolds, and growth factors are being developed to promote nerve regeneration and repair after injury or surgery.
- Stem Cell Therapy: Ongoing research into stem cell therapy aims to repair damaged brain and spinal tissue by regenerating neurons and supporting neural connections.
13. Liquid Biopsies and Molecular Profiling
- Neurosurgeons are leveraging liquid biopsies, which analyze circulating tumor DNA (ctDNA) in blood or cerebrospinal fluid, to detect and monitor brain tumors. This non-invasive approach provides insights into tumor genetics, aiding in personalized treatment plans.
- Molecular Profiling: Identifying genetic mutations and molecular characteristics of brain tumors (e.g., gliomas) allows for more targeted and personalized therapies, such as immunotherapy or targeted molecular inhibitors.
14. Cerebrospinal Fluid (CSF) Shunt Technologies
- New advancements in shunt systems used to treat hydrocephalus include programmable shunts with pressure sensors that adjust the flow of CSF based on the patient’s needs. This helps reduce complications such as under- or over-drainage.
Benefits for the Patient
At our Neurosys Multispeciality Center, we perform several key procedures including Craniotomy, which is primarily for the excision of brain tumors; V-P Shunt Surgery for treating hydrocephalus; surgeries for epilepsy; and operations targeting brain stem glioma. Beyond these, we offer a range of other neurosurgical services. If you have any questions that are not answere, please contact us through our Contact Us or Book your Appointment.
